Part 1 – This will be another two-parter, as glaucoma is pretty complicated and long as well!
“Hey doc, can I get some pot for my glaucoma??”
You know, it’s funny how often I still get this question. The short answer is no. The long answer is “No and here’s why…” which can be a long answer. I’ll try to keep it to be a medium answer though. So let’s talk about glaucoma, one of the least understood and most confused conditions by patients.
What is glaucoma? That’s a great question that a lot of patients ask me on a near daily basis. Some patients have heard of it thinking it has to do with high eye pressure. While you’re not wrong for thinking that, you’re not entirely correct either.
Glaucoma is a condition characterized by nerve damage to the back of the eye. This nerve damage is painless and in most cases symptomless early on in the disease. As time goes on, if someone is unchecked, they can develop peripheral (side vision) loss that can work its way towards the middle of the vision and eventually cause central vision loss.
Notice how I didn’t mention eye pressure in that definition? That’s because there are so many kinds of glaucoma, that high eye pressure isn’t always a defining feature! With just a quick tally off the top of my head, I wrote out about 15 different kinds of glaucoma. Many of them can start off with normal eye pressure and eventually lead to high pressure, but not all of them.
One of the biggest difficulties in treating glaucoma is that patients aren’t aware of symptoms and don’t realize how serious the condition can be until it’s too late. I remember a patient I saw a few years ago who came in and said, “I was told I had cataracts 5 years ago. They said I should come back, but I didn’t think it was important, so I didn’t go back. I just want to see if they’re worse or not.”
When I dilated her eyes, I could tell she had no sign of cataracts whatsoever. In fact, she was seeing 20/20 in each eye and overall looked to be in good health. But when I was able to see the back of her eye (her retina and optic nerve), I noted that her left eye’s optic nerve was much larger than the right eye.
It was significant enough that I sat back and told her that unfortunately she misunderstood and was told it she was a glaucoma suspect 5 years ago and I fear that 5 years of going without treatment had potentially caused significant vision loss. When we tested her visual fields, we found she was missing a significant portion of her upper visual field, despite her 20/20 vision!
Glaucoma Suspects and Risk Factors
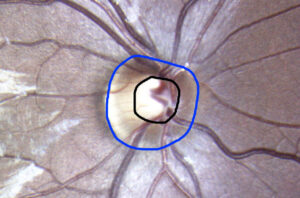
So what goes into determining if someone is a glaucoma suspect or has glaucoma? Well first and foremost we look at the appearance of the optic nerve. The optic nerve is shaped kind of like a donut with a donut hole in it. The photos below are a zoomed in, blown up picture of my own optic nerve.
If you take a look at first photo, you’ll see it unedited, the way I see patient’s optic nerves when I look inside their eye. The second photo is an edited version where I drew around it. The black circle is to illustrate the “donut hole,” while the blue circle is outlining “the donut.” We grade this based on the ratio of donut to donut hole.
The larger the donut hole, the more concerned we are for someone to have glaucoma. If there are changes in someone’s optic nerve appearance, they can often be subtle and difficult to spot on a year to year basis. This is why photographs can be so important in early cases to monitor for more subtle changes. It’s one of the biggest reasons we recommend the wellness photos for patients who have no underlying eye pathology.

During an annual eye health examination, the other measurement we take on all patients is their eye pressure, also known as their intraocular pressure (IOP). The IOP measurement can be taken in many different ways. One of these methods is the universally dreaded “air puff test.”
While that method is commonly used, it’s one we at Mt. View EyeCare rarely use anymore, as we have better, alternative methods that are much easier for patients to handle. The method we commonly use is one where a little instrument is held up in front of your eye. You often feel a little tickle on your eyelashes, but that’s about it. It’s quick and painless and gives good, consistent results in most cases.
The gold standard method does require that we use anesthetic and dye to measure a patient’s IOP, but we reserve that method more for glaucoma patients or high risk suspects that we want to get more exact pressure measurements on.
What other risk factors are there?
Well, I’m glad you asked!
Besides optic nerve size and eye pressure, there can be a lot of other factors depending on the type of glaucoma.
One of the most significant universal risk factors is family history. The strongest link is typically a twin, then a sibling, then mom, then dad, then everyone else. Your genetics play a big role in what conditions you may eventually develop and glaucoma is certainly not exempt!
Age is another risk factor we consider. While glaucoma typically occurs in patients in their 60s or 70s (and up), patients risk factors often begin to increase around the age of 40. That doesn’t mean that you can’t develop glaucoma in your 20s or 30s, but it does mean it’s less common for it to occur. There are even cases where infants are born with glaucoma or children develop it early in childhood.
Other systemic conditions are often commonly associated as well. Patients with diabetes are 5x more likely to develop glaucoma and patients with sleep apnea are 2.5x more likely to develop glaucoma than those without those conditions. In terms of your eyes, patients who are nearsighted are often more prone to the development of some types of glaucoma, while farsightedness can put you at risk for others.
As I mentioned before, there are a lot of subtypes of glaucoma. You see, glaucoma is the umbrella term with all the different types falling underneath that umbrella. There’s what we call primary open angle glaucoma (the most common type), but there is also normal pressure glaucoma (this is where there is still glaucoma damage to the eye, but the eye pressures are in the normal range). There’s two other kinds that can occur when patients are losing pigment from their iris or one where their lens is shedding an outer layer. These two subtypes can lead to the drain pipes inside the eye where the fluid normally leaves the eye becoming clogged up and leading to an increase in pressure and therefore glaucoma.
Finally, there are some medications that put you at higher risk for developing certain types of glaucoma as well. Steroids are a good, common example that (oral or topical) can increase your risk of your eye pressure increasing. There are many other medications that can put you at risk, but these are medications we watch for when we ask for your most recent medication list.
While that’s just some of the risk factors, there are so many more! So this post doesn’t end up getting to be too long (it’s already longer than I intended), I’ll split this into two posts as well. The next blog will consist of how we monitor glaucoma patients and glaucoma suspects, as well as some of the treatment options and why marijuana is not a viable treatment option!
Thanks for reading!
Dr. Nick